The first babies conceived with a sperm-injecting robot have been born
Last spring, engineers in Barcelona packed up the sperm-injecting robot they’d designed and sent it by DHL to New York City. They followed it to a clinic there, called New Hope, where they put the instrument back together, assembling a microscope, a mechanized needle, a tiny petri dish, and a laptop.
Then one of the engineers, with no real experience in fertility medicine, used a Sony PlayStation 5 controller to position a robotic needle, which, eyeing a human egg through a camera, then moved forward on its own, penetrating the egg and dropping off a single sperm cell. Altogether, the robot was used to fertilize more than a dozen eggs.
The result of the procedures, say the researchers, were healthy embryos—and now two baby girls, who they claim are the first people born after fertilization by a “robot.”
“I was calm. In that exact moment, I thought, ‘It’s just one more experiment,’” says Eduard Alba, the student mechanical engineer who commanded the sperm-injecting device.
The startup company that developed the robot, Overture Life, says its device is an initial step toward automating in vitro fertilization, or IVF, and potentially making the procedure less expensive and far more common than it is today.
Right now, IVF labs are multimillion-dollar affairs staffed by trained embryologists who earn upwards of $125,000 a year to delicately handle sperm and eggs using ultra-thin hollow needles under a microscope.
But some startups say the entire process could be carried out automatically, or nearly so. Overture, for instance, has filed a patent application describing a “biochip” for an IVF lab in miniature, complete with hidden reservoirs containing growth fluids, and tiny channels for sperm to wiggle through.
“Think of a box where sperm and eggs go in, and an embryo comes out five days later,” says Santiago Munné, the prize-winning geneticist who is chief innovation officer at the Spanish company. He believes that if IVF could be carried out inside a desktop instrument, patients might never need to visit a specialized clinic, where a single attempt at getting pregnant can cost $20,000 in the US. Instead, he says, a patient’s eggs might be fed directly into an automated fertility system at a gynecologist’s office. “It has to be cheaper. And if any doctor could do it, it would be,” says Munné.
MIT Technology Review identified a half-dozen startups with similar aims, with names like AutoIVF, IVF 2.0, Conceivable Life Sciences, and Fertilis. Some have roots in university laboratories specializing in miniaturized lab-on-a-chip technology.
So far, Overture has raised the most: about $37 million from investors including Khosla Ventures and Susan Wojcicki, the former CEO of YouTube.
More babies
The main goal of automating IVF, say entrepreneurs, is simple: it’s to make a lot more babies. About 500,000 children str born through IVF globally each year, but most people who need help having kids don’t have access to fertility medicine or can’t pay for it.
“How do we go from half a million babies a year to 30 million?’” wonders David Sable, a former fertility doctor who now runs an investment fund. “You can’t if you run each lab like a bespoke, artisanal kitchen, and that is the challenge facing IVF. It’s been 40 years of outstanding science and really mediocre systems engineering.”
While an all-in-one fertility machine doesn’t yet exist, even automating parts of the process, like injecting sperm, freezing eggs, or nurturing embryos, could make IVF less expensive and eventually support more radical innovations, like gene editing or even artificial wombs.
But it won’t be easy to fully automate IVF. Just imagine trying to make a robot dentist. Test-tube conception involves a dozen procedures, and Overture’s robot so far performs only one of them, and only partially.
“The concept is extraordinary, but this is a baby step,” says Gianpiero Palermo, a fertility doctor at Weill Cornell Medical Center who is credited with developing the fertilization procedure known as intracytoplasmic sperm injection, or ICSI, in the 1990s. Palermo notes that Overture’s researchers still relied on some manual assistance for tasks like loading a sperm cell into the injector needle. “This is not yet robotic ICSI, in my opinion,” he says.
Other doctors are skeptical that robots can, or should, replace embryologists anytime soon. “You pick up a sperm, put it in an egg with minimal trauma, as delicately as possible,” says Zev Williams, director of Columbia University’s fertility clinic. For now, “humans are far better than a machine,” he says.
His center did develop a robot, but it has a more limited aim: dispensing tiny droplets of growth medium for embryos to grow in. “It’s not good for the embryos if the drop size differs,” says Williams. “Creating the same drops over and over again—that is where the robot can shine.” He calls it a “low risk” way to introduce automation to the lab.
Micro cradles
One obstacle to automating conception is that so-called microfluidics—another name for lab-on-a-chip technology—hasn’t lived up to its hype.
Jeremy Thompson, an embryologist based in Adelaide, Australia, says he’s spent his career figuring out “how to make the lives of embryos better” as they grow in laboratories. But until recently, he says, his tinkering with microfluidic systems yielded an unambiguous result: “Bollocks. It didn’t work.” Thompson says IVF remains a manual process in part because no one wants to trust an embryo—a potential person—to a microdevice where it could get trapped or harmed by something as tiny as an air bubble.
A few years ago, though, Thompson saw images of a minuscule Eiffel Tower, just one millimeter tall. It had been made using a new type of additive 3D printing, in which light beams are aimed to harden liquid polymers. He decided this was the needed breakthrough, because it would let him build “a box or a cage around an embryo.”
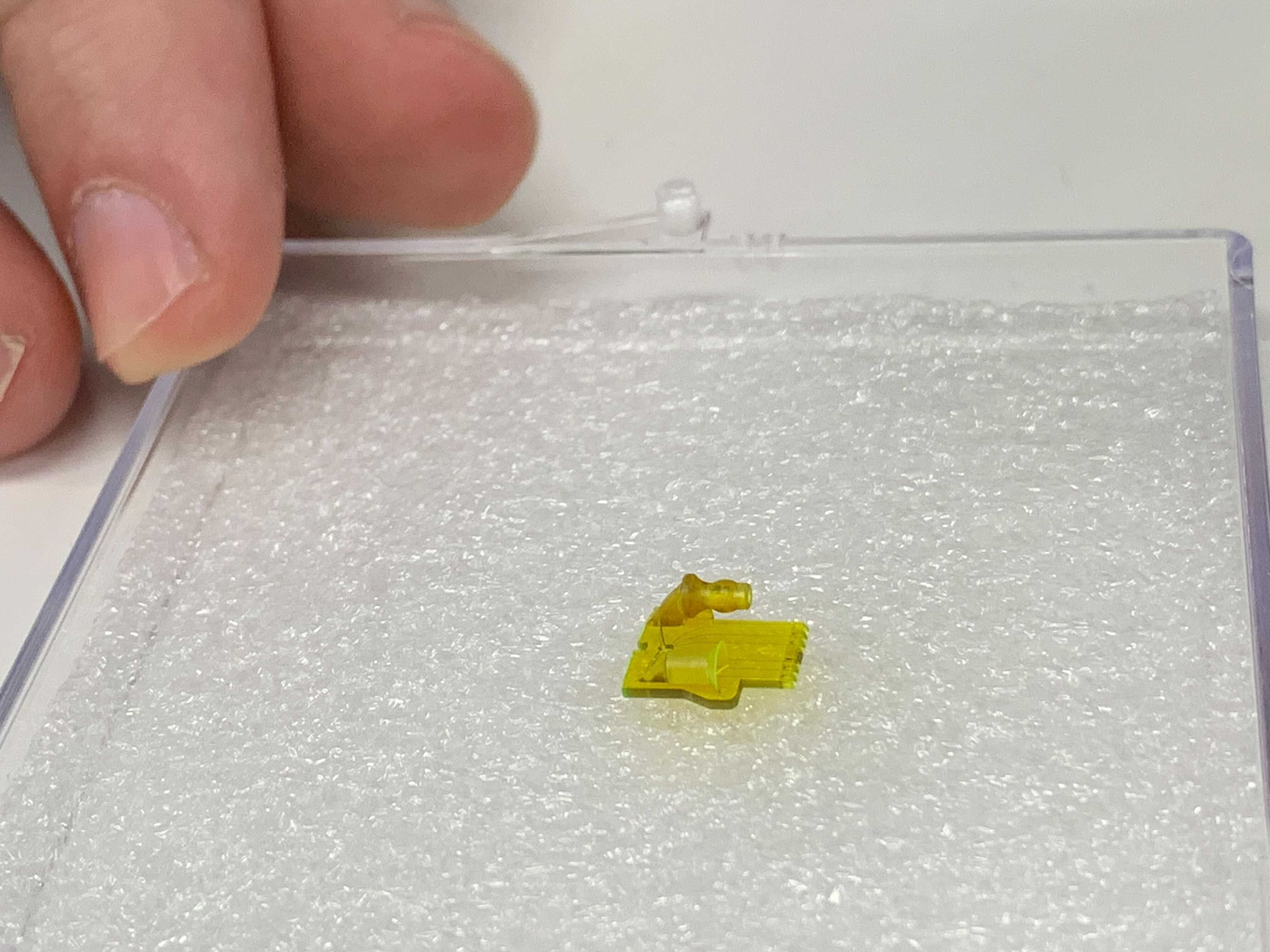
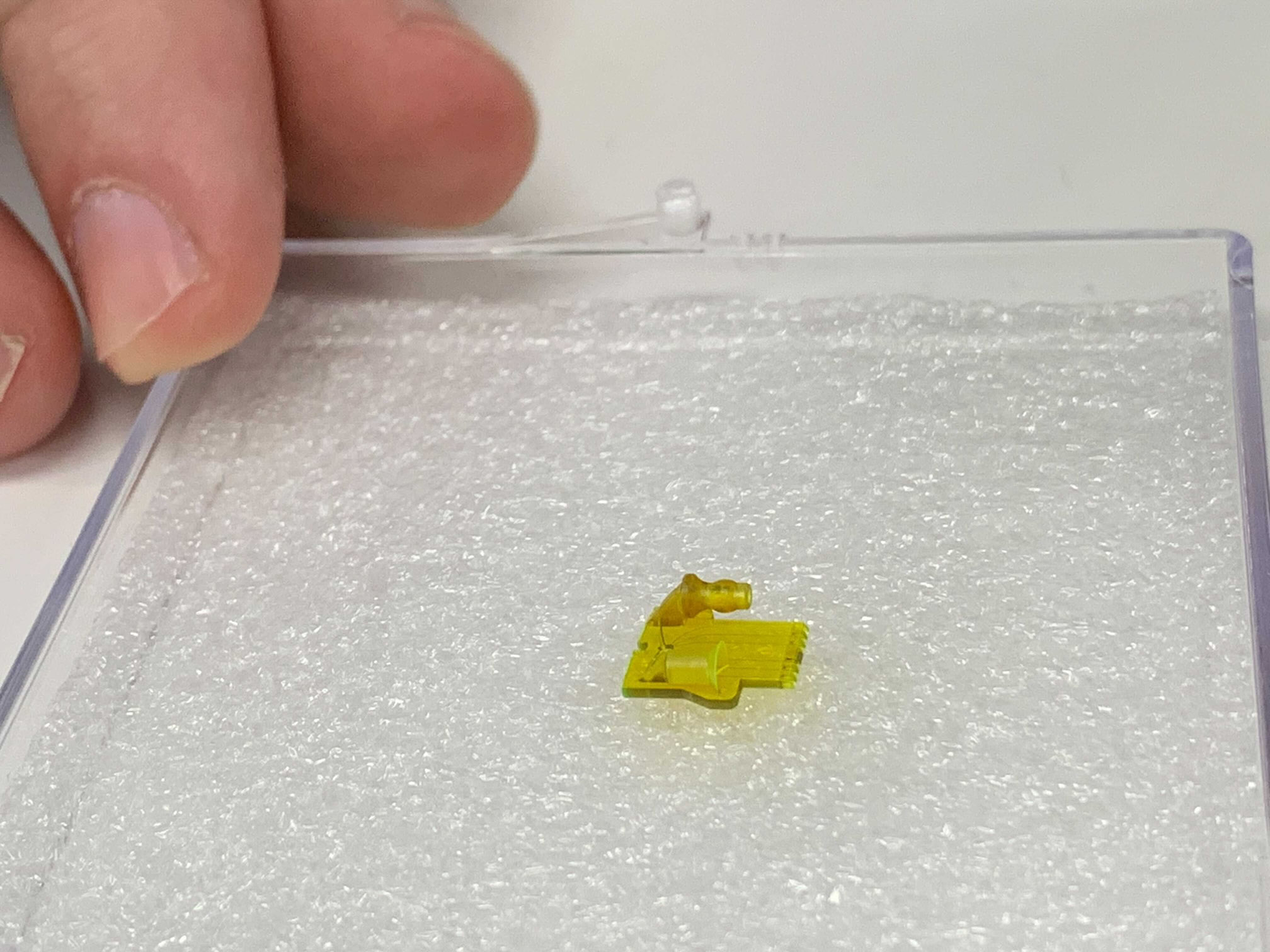
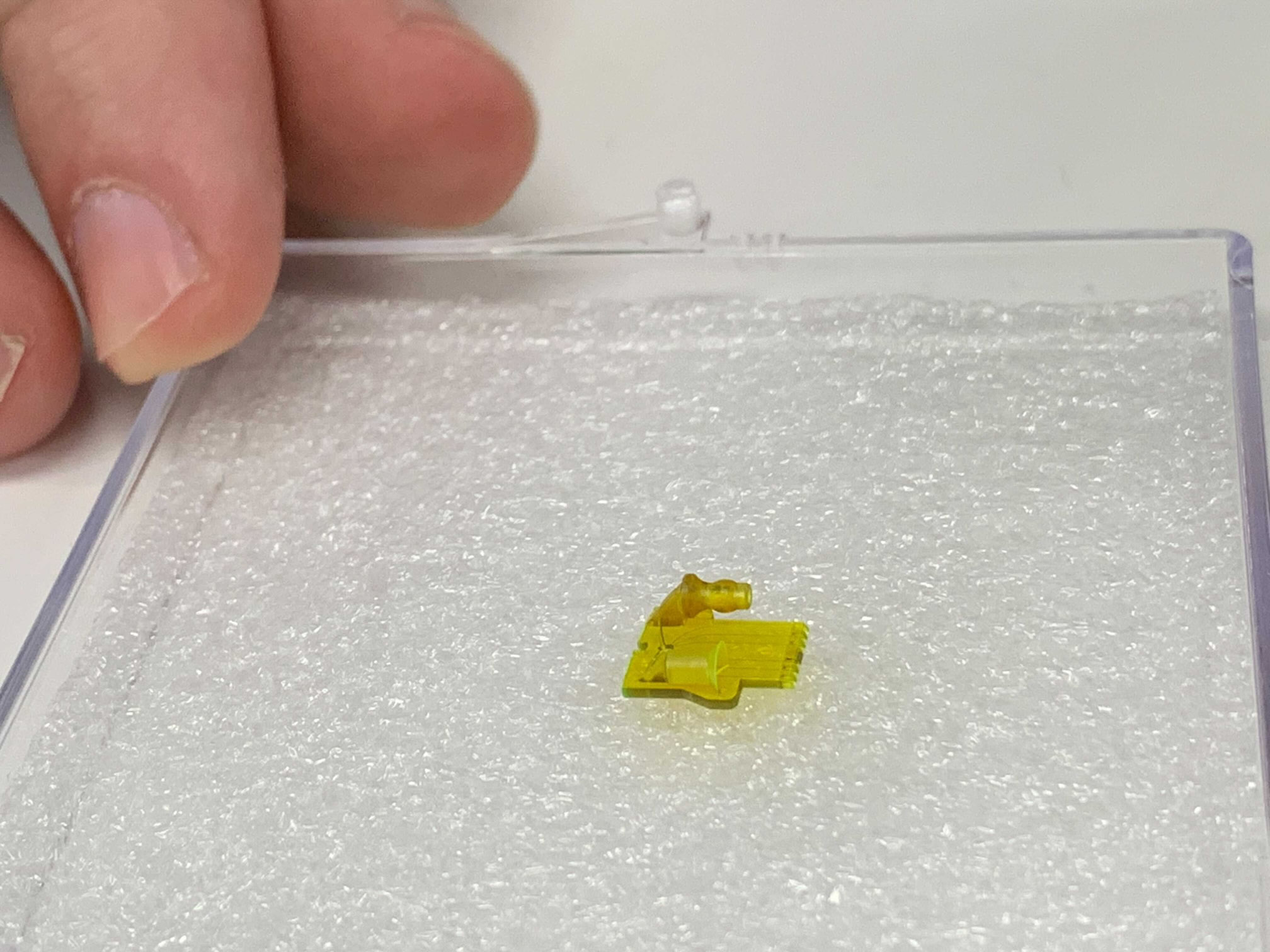
Since then, a startup he founded, Fertilis, has raised a couple of million dollars to print what it calls see-through “pods” or “micro-cradles.” The idea is that once an egg is plopped into one, it can be handled more easily and connected to other devices, such as pumps to add solutions in minute quantities.
Inside one of Fertilis’s pods, an egg sits in a chamber no larger than a bead of mist, but the container itself is large enough to pick up with small tongs. Fertilis has published papers showing it can flash-freeze eggs inside the cradles and fertilize them there, too, by pushing in a sperm with a needle.
A human egg is about 0.1 millimeters across, at the limit of what a human eye can see unaided. Right now, to move one, an embryologist will slurp it up into a hollow needle and squirt it out again. But Thompson says that once inside the company’s cradles, eggs can be fertilized and grow into embryos, moving through the stations of a robotic lab as if on a conveyor belt. “Our whole story is minimizing stress to embryos and eggs,” he says.
Thompson hopes someday, when doctors collect eggs from a woman’s ovaries, they’ll be deposited directly into a micro-cradle and, from there, be nannied by robots until they’re healthy embryos. “That’s my vision,” he says.
MIT Technology Review found one company, AutoIVF, a spinout from a Massachusetts General Hospital–Harvard University microfluidics lab, that has won more than $4 million in federal grants to develop such an egg-collecting system. It calls the technology “OvaReady.”
Egg collection happens after a patient is treated with fertility hormones. Then a doctor uses a vacuum-powered probe to hoover up eggs that have ripened in the ovaries. Since they’re floating in liquid debris and encased in protective tissue, an embryologist needs to manually find each one and “denude” it by gently cleaning it with a glass straw.
An AutoIVF executive, Emre Ozkumur, declined to discuss the project—the company wants to “stay under the radar a little bit longer,” he says—but its grant and patent documents suggest it is testing a device that can spot and isolate eggs and then automatically strip them of surrounding tissue, perhaps by swishing them through something that resembles a microscopic cheese grater.
Sperm tracker
Once an egg is in hand, doctors need to match it with a sperm cell. To help them pick the right one, Alejandro Chavez-Badiola, a fertility doctor based in Mexico, started a company, IVF 2.0, that developed software to rank and analyze sperm swimming in a dish. It’s similar to computer-vision programs that track sports players as they run, collide, and switch directions on a pitch.
The job is to identify healthy sperm by assessing their shape and seeing how well they swim. “Motility,” says Chavez-Badiola, “is the ultimate expression of sperm health and normality.” While a person can only keep an eye on a few sperm at one time, a computer doesn’t face that limit. “We humans are good at channeling our attention to a single point. We can assess five or 10 sperm, but you can’t do 50,” says Chavez-Badiola.
His IVF clinic is running a head-to-head study of human- and computer-picked sperm, to see which lead to more babies. So far, the computer holds a small edge.
“We don’t claim it’s better than a human, but we do claim it’s just as good. And it never gets tired. A human has to be good at 8 a.m., after coffee, after having an argument on the phone,” he says.
Chavez-Badiola says such software will be “the brains to command future automated labs.” This year, he sold the rights to use his sperm-tracking program to Conceivable Life Sciences, another IVF automation startup being formed in New York where Chavez-Badiola will act as chief product officer. Also joining the company is Jacques Cohen, a celebrated embryologist who once worked at the British clinic where the first IVF baby was born in 1978.
Conceivable plans to create an “autonomous” robotic workstation that can fertilize eggs and cultivate embryos, and it hopes to demonstrate all the key steps this year. But Cohen allows that automation could take a while to become reality. “It will happen step by step,” he says. “Even things that seem obvious take 10 years to catch on, and 20 to become routine.”
The investors behind Conceivable think they can cash in by expanding the use of IVF. It’s nearly certain that the IVF industry could grow to five or 10 times its current size. In the US, fewer than 2% of kids are born this way, but in Denmark, where the procedure is free and encouraged, the figure is near 10%.
“That is the true demand,” says Alan Murray, an entrepreneur with a background in software and co-working spaces who cofounded Conceivable with his business partner, Joshua Abram. “The challenge is that these wonderful rich and eccentric countries can do it, but the rest of the world cannot. But they have demonstrated the true human need,” he says. “What they have done with money, we need to do with technology.”
Murray estimates the average IVF baby in the US costs $83,000 if you include failed attempts, which are common. He says his company’s objective is to lower the cost by 70%, something he says can happen if success rates increase.
But it’s not a given that robots will reduce the cost of IVF or that any savings will be passed on to patients. Rita Vassena, an advisor to Conceivable and chief science officer at Fecundis, a fertility science company, says the field has a history of introducing innovations without appreciably increasing pregnancy rates. “The trend [is] toward piling up tests and technologies … rather than a true effort to lower access barriers,” she says.
Future worlds
Last fall, the researchers at Overture and doctors at New Hope published a description of their work with the robot, claiming that two patients had become pregnant. Both those children have now been born, says Jenny Lu, the egg donation coordinator at New Hope. MIT Technology Review was able to speak to the father of one of the children.
“It’s wild, isn’t it,” said the father, who asked to remain anonymous. “They said up until now it had always been done manually.”
He said he and his partner had tried IVF several times before, without success. Both cases of robot injection involved donor eggs, which were provided to the patients for free (they can cost $15,000 otherwise). In each case, after being fertilized and grown into embryos, they were implanted in the uterus of the patient.
Donor eggs are most often used when a patient is older, in her 40s, and can’t get pregnant otherwise.
Since automation won’t directly solve the problem of aging eggs, an IVF lab-in-a-box won’t fix this intractable reason that fertility treatments fail. However, automation could let doctors begin precisely measuring what they do, allowing them to fine-tune their procedures. Even a small increase in success rates could mean tens of thousands of extra babies every year.
Kathleen Miller, chief scientist of Innovation Fertility, a chain of clinics in the southern US, says her centers are now using computer-vision systems to study time-lapse videos of growing embryos and trying to see if any data explain why some become babies and others don’t. “We’re putting it into models, and the question is ‘Tell me something I don’t know,’” she says.
“We’re going to see an evolution of what an embryologist is,” Miller predicts. “Right now, they are technicians, but they’re going to be data scientists.”
For some proponents of IVF automation, an even wilder future awaits. By giving over conception to machines, automation could speed the introduction of still-controversial techniques such as genome editing, or advanced methods of creating eggs from stem cells.
Although Munné says Overture Life has no plans to modify the genetic makeup of children, he allows it would be a simple matter to use the sperm-injecting robot for that purpose, since it could dispense precise amounts of gene-editing chemicals into an egg. “It should be very easy to add to the machine,” he says.
Even more speculative technology is on the horizon. Fertility machines could gradually evolve into artificial wombs, with children gestated in scientific centers until birth. “I do believe we are going to get there,” says Thompson. “There is credible evidence that what we thought was impossible is not so impossible.”
Others imagine that robots could eventually be shot into outer space, stocked with eggs and sperm held in a glassy state of stasis. After a thousand-year journey to a distant planet, such machines might boot up and create a new society of humans.
It’s all part of the goal of creating more people, and not just here on Earth. “There are people thinking that humankind should be an interplanetary species, and human lifetimes are not going to be enough to reach out to these worlds,” says Chavez-Badiola. “Part of the job of a scientist is to keep dreaming.”